
Healthcare organizations are facing unprecedented operational challenges in the post-pandemic era, particularly within revenue cycle management. High attrition rates among call center staff—often reaching 30% to 45%—combined with mounting pressure to reduce costs and enhance patient satisfaction, have left many providers struggling to maintain efficiency and service standards.
Concurrently, technological advancements in artificial intelligence (AI) offer transformative potential, particularly through the deployment of Digital Employees.
This white paper by Smart Source, LLC introduces a powerful solution: the integration of Conversational AI-powered Digital Employees into the healthcare revenue cycle. Unlike generative AI, which poses compliance risks due to potential inaccuracies (“hallucinations”), Conversational AI provides controlled, regulation-compliant interaction with patients while maintaining contextual awareness and memory—key for meeting HIPAA, Privacy, and PCI compliance requirements.
The financial implications of underperforming call operations are substantial. One case study highlighted an abandoned call rate of 8%, equating to an estimated $2.2 million in unrealized net revenue annually for a specialty practice.
Moreover, approximately 80% of calls are repetitive in nature—such as confirmations, cancellations, and information requests—which are ideal for automation. Replacing or supplementing staff with digital employees can not only reduce these inefficiencies but also increase revenue and lower operational costs, including training and benefits.
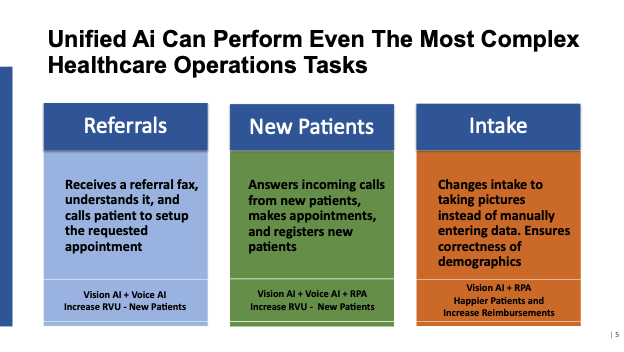
Smart Source's Digital Employee solution leverages a unified AI toolkit—consisting of Speech AI, Vision AI (OCR), and Robotic Process Automation (RPA)—to automate high-volume, rules-based tasks. These include appointment scheduling, insurance verification, reminders, outbound screening campaigns, and payment collection. The system is customizable, integrates with major EHR systems (e.g., Epic, Cerner, Athena), and can mirror an organization’s unique vernacular and workflows.
Key benefits include:
Smart Source emphasizes a disciplined implementation approach, aligned with the U.S. Navy SEALs’ philosophy of “Slow is smooth, smooth is fast.” By advocating a deliberate, feedback-driven rollout, healthcare organizations can avoid common pitfalls and realize sustainable, scalable improvements.
In a rapidly evolving healthcare landscape, Digital Employees are no longer an optional enhancement—they are a strategic imperative. Smart Source, LLC stands ready to demonstrate the value of its solution, empowering healthcare organizations to thrive through innovation, compliance, and operational excellence.
Before we review digital employee features and capabilities it is important that we differentiate between conversational AI and generative AI as it applies to healthcare.
Healthcare organizations must strictly adhere to government regulations on many levels. One, based on the healthcare revenue cycle, is compliance. This is broken down into several categories.
HIPAA stands for the Health Insurance Portability and Accountability Act of 1996. It is a U.S. federal law designed to protect sensitive patient health information from being disclosed without the patient's consent or knowledge.
In healthcare, privacy refers to an individual’s right to control the access, use, and disclosure of their personal health information (PHI). It is a foundational principle in medical ethics and legal standards, ensuring that patients can trust healthcare systems with their most sensitive data.
PCI compliance refers to adhering to the Payment Card Industry Data Security Standard (PCI DSS)—a set of requirements designed to ensure that all organizations that store, process, or transmit credit card information maintain a secure environment.
It is essential for businesses of all sizes that handle payment card data, including hospitals, clinics, or any healthcare providers that accept credit or debit card payments.
Given these requirements it is essential that all information and data flows adhere to these compliance standards.
Conversational AI uses advanced natural language processing (NLP) and machine learning to understand context across multiple interactions. It remembers previous conversations, allowing for more personalized and fluid experiences.
Traditional chatbots usually operate on scripted flows and do not retain memory across sessions — they often treat each query as a separate, isolated event.
Natural Language Processing (NLP) Capabilities
Conversational AI can interpret complex language, including slang, accents, typos, and varied sentence structures. It understands intent and handles ambiguity better.
Chatbots often require users to use predefined commands or button selections, leading to frustration if users stray from the script.
Many conversational AI solutions can perform sentiment analysis, adapting tone and responses based on whether a user is happy, angry, or confused.
Traditional chatbots generally cannot detect emotions, leading to tone-deaf or insensitive responses.

The following chart provides the differences between conversational AI and generative AI and what each excels at doing. The major concern with generative AI in the healthcare revenue cycle is compliance with HIPPA, Privacy and PCI compliance.
It is suggested that controls be tight and well defined when working within the healthcare revenue cycle and conversational AI provides those controls.
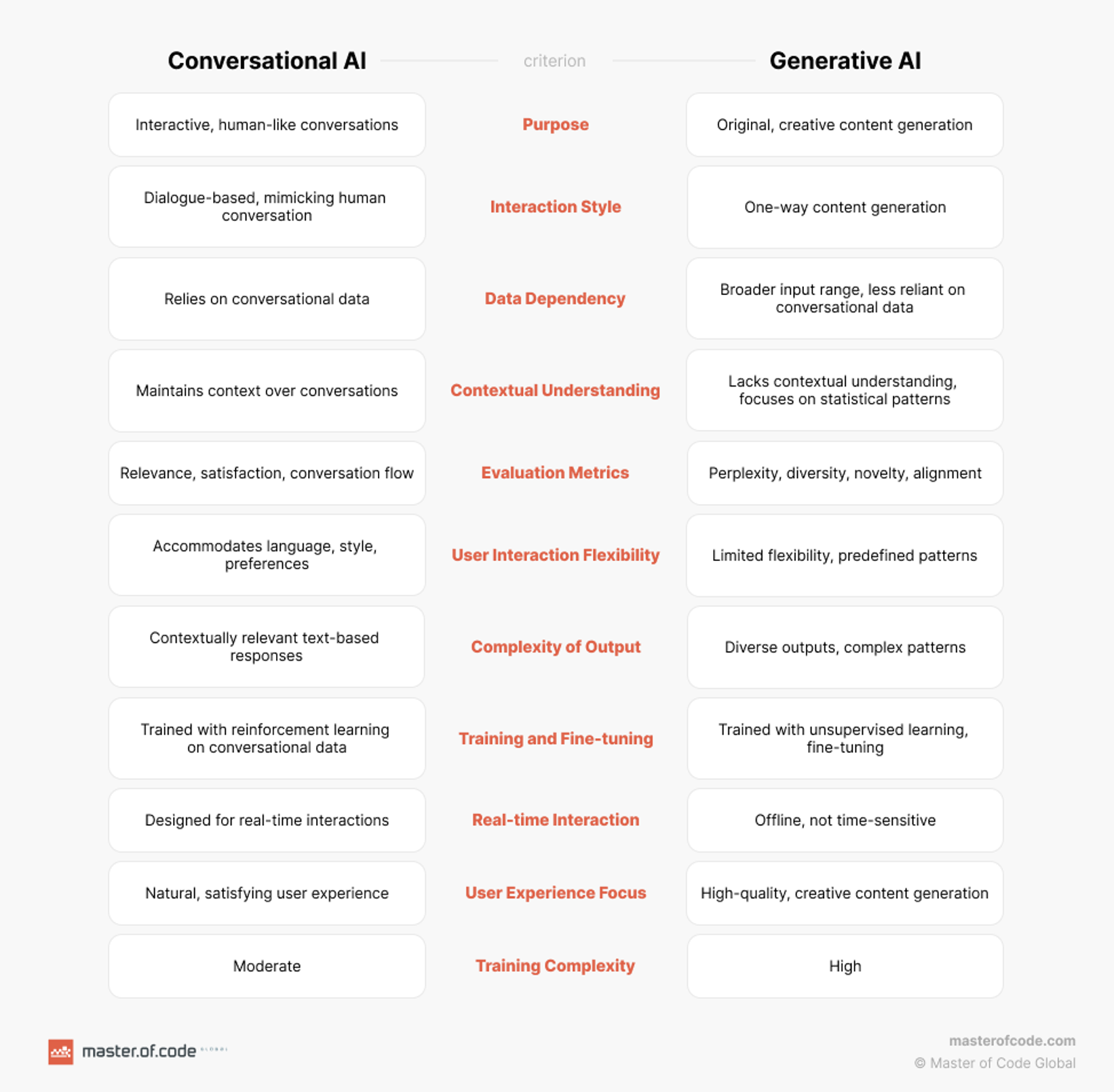
As you can see from this chart the revenue cycle activities are much more controlled and well defined using conversational AI rather than generative AI. As our goal is task completion, consistency, compliance, and efficiency, conversational AI is superior.
If your goal is creative, human-like dialogue for exploration, brainstorming, or storytelling, generative AI chatbots shine.
There is also a very real concern, and it has been seen in many “quick to market” products using generative AI, what are called “hallucinations” or made-up incorrect
responses. With the focus on compliance these issues must be addressed in the development of any product that is introduced to the healthcare revenue cycle system.
One of the significant challenges that healthcare revenue cycle operations encounter is that of answering phone calls and making outbound phone calls. Post pandemic attrition rates among call centers and departments who manage inbound and outbound calls are between 30% and 45%.
This inability has led to:
The primary factors that result in this attrition rate of 30% - 45% are high stress and burnout. The ongoing demand to meet specific metrics lead to this stress and burnout. This seems to be a never-ending cycle of turnover due to the inability to find and replace staff. The cost to train a new staff member is approximately 20% of their salary.
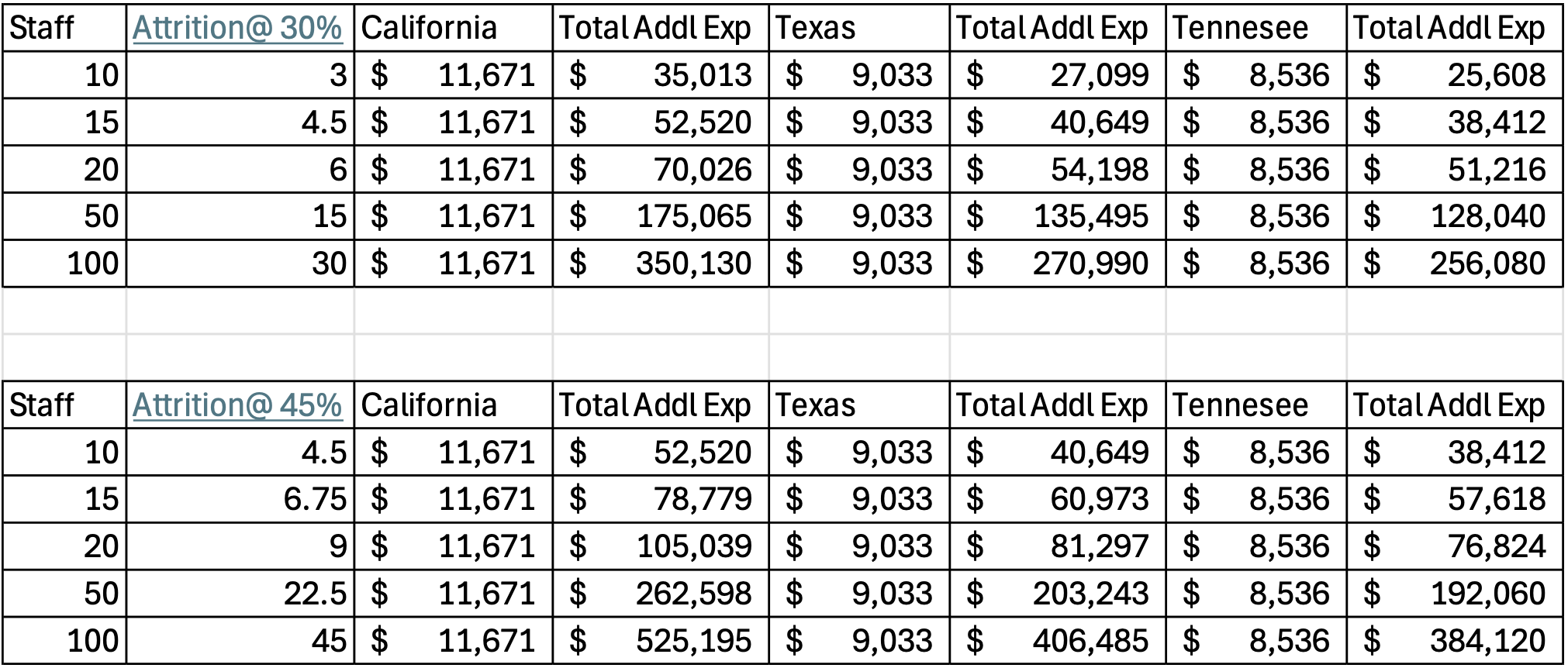
In California the average healthcare call center salary is $58,355 or an additional $11,671 in training costs. In Texas the average healthcare call center salary is $45,169 or an additional $9,033 in training costs. In Tennessee the average healthcare call center salary is $42,683 or an additional $8,536 in training costs. These numbers do not include benefits that can range from 10% - 45%. (source: Indeed, Salary, Job Search)
The two charts below indicate the amount of additional costs that must be budgeted to accommodate the expense of training new staff.
This does not consider:
Erlang C is a formula used to calculate how many agents are needed to handle incoming calls. It assumes calls arrive randomly, agents work steadily, and everyone waits in line until their turn. However, it doesn’t consider customers who might hang up if the wait gets too long. (source, Olaf Jacobson, Understanding Erlang C, Erlang A, and Simulation for Workforce Management Soon, January 15, 2025)
From a practical standpoint it calculates the number of FTE’s required to manage metrics at expected service levels. One mistake that is often made in budgeting for call centers or revenue cycle departments that manage inbound and outbound calls, is that they do not consider that staff have approximately 10% -15% of their time away from the office for appointments, sick time, vacations, etc.
Given the requirements for managing the service levels to targets it is necessary to budget those additional FTE’s to meet the requirements of the operations.
There are number of “arguments” either way when it comes to determining what are the “correct” metrics are for call centers or departments. These vary by minor percentages; however, the goal is to be able to handle all calls as quickly as possible with a positive result for the patient, department or clinician.
Healthcare call centers often handle complex and sensitive inquiries, necessitating tailored benchmarks:
First Call Resolution (FCR): 75%–85%
Average Handle Time (AHT): 6–8 minutes
Call Abandonment Rate: 3%–5%
Average Speed of Answer (ASA): Approximately 3 minutes 22 seconds
Hold Time: Around 50 seconds
Abandonment Rate: Approximately 7%
(source: Nubitel – Contact Center Insights – Dang Tin Wai, March 9, 2025)
While all of these are important, the focus should be on abandoned call rates that impact on the other metrics as well as lost revenue, additional expenses and decreased satisfaction with all customers.
One of our clients, as part of our due diligence, provided us with their call volumes for one year. Based on our initial assessment we determined that they had an abandoned call rate of 8%.
This was a specialty practice that provided a variety of services including office visits, biopsies, minor surgery and some cosmetic procedures. For the purposes of illustration, we used the Medicare fee schedule for a blend of new and returning patients using HCPCS codes 99205 and 99213 to come up with an average of $155.
Based on their current abandoned call rate of 8% they could potentially realize an additional $2.2 million in net revenue. The chart shows the variation in additional revenue based on the abandoned call rate.
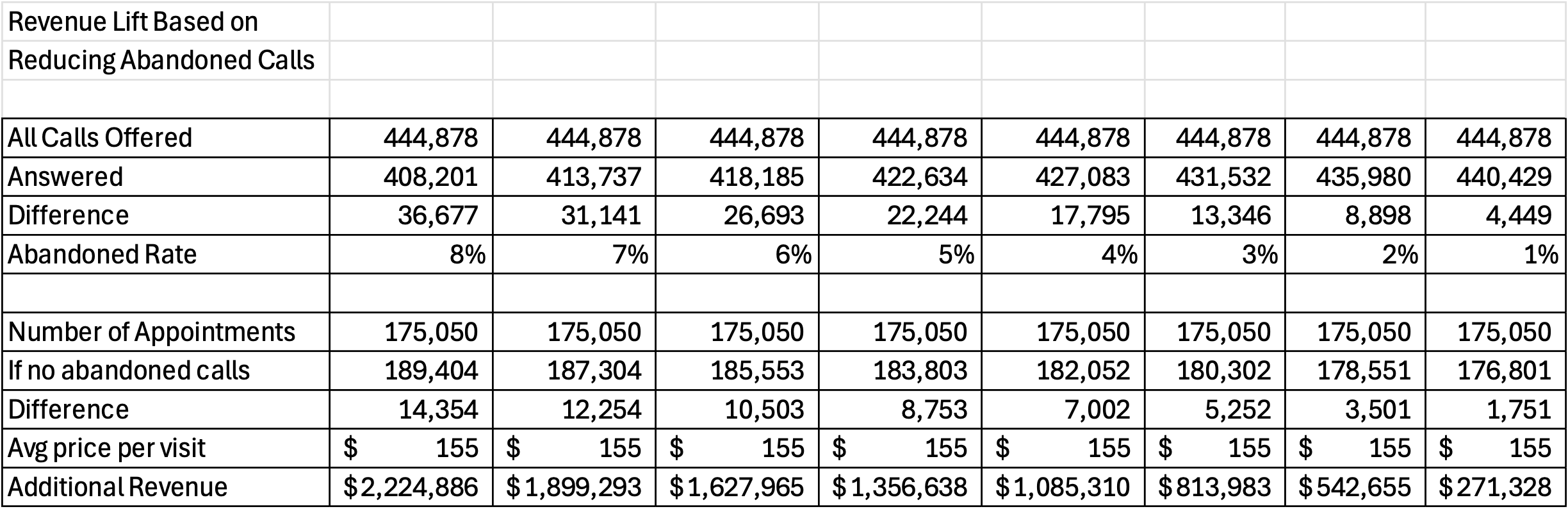
These are routine office visits and do not reflect the higher priced procedures, Imaging, Cardiology, Oncology, etc. Pricing for these procedures is significantly higher and would impact on additional revenue at a much higher level.
Staffing Implications
Of the 408,201 calls that were answered, 233,151 were calls to cancel, confirm, reschedule or requests for information. Except for a request for information that could be handled by a staff member, all the other calls are repetitive tasks.
Of the 233,151, 21%, or 46,630 would be handled by a staff member, but the other 186,521 were answered by staff to perform a repetitive task.
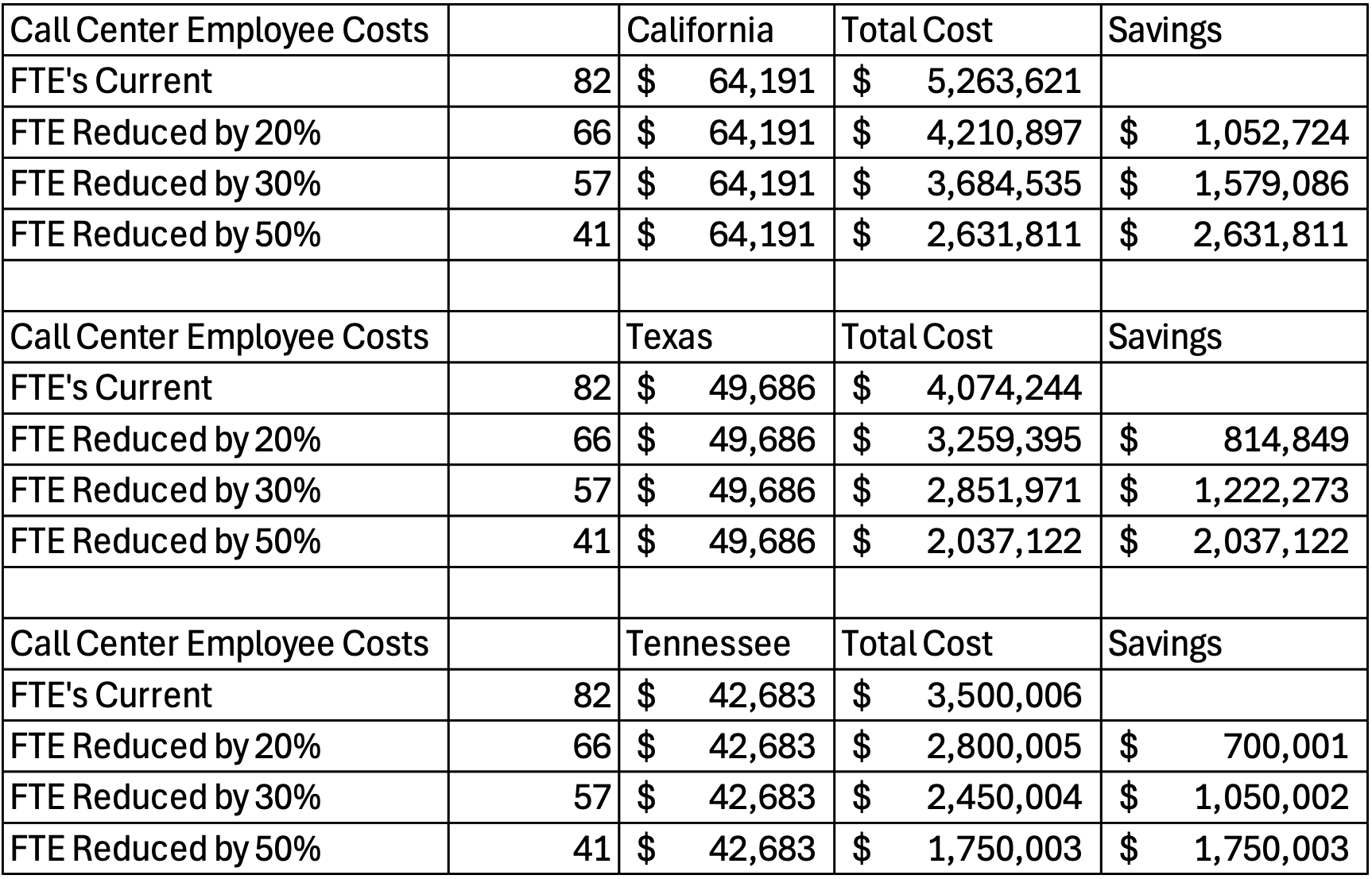
For a comparison of costs between states we took the current staff available to manage the current calls, at 82 and reduced them by 50%, adding a 10% benefit package. Again, we used California, Texas and Tennessee to use similar comparative information and calculated the savings if staffing could be reduced and revenue increased without further costs.
When viewed on a day-to-day basis, the abandoned call rates, staffing and budgeting are considered part of the process. However, when you annualize the potential net revenue impact as well as the staffing implications the potential increase in net revenue and the decrease in costs are significant.
As in days past, when we migrated from mainframe computers to desktop computers to laptop computers and then to tablets, technology continues to evolve at an ever-rapid pace.
The “Rise” of Artificial Intelligence
In a recent article in the Harvard Business Review, it stated that:
“AI agents are fast becoming much more than just sidekicks for human workers. They’re becoming digital teammates—an emerging category of talent. To get the most out of these new teammates, leaders in HR and procurement will need to start developing an operational playbook for integrating them into hybrid teams and a workforce strategy.” (source: Agentic AI Is Already Changing the Workforce, by Jen Stave, Ryan Kurt and John Winsor May 22, 2025 – HBR Digital)
With this thought in mind, we would like to look at digital teammates and applications that support them. What follows is a discussion of the various AI applications that are part of the healthcare revenue cycle and how the integration of various AI applications cannot support the various functions.
AI are “intelligent” program applications that can work independently or in concert with other programs to produce desired results.
The three basic “intelligent” applications used in the operational aspects of the healthcare revenue cycle are:
We will define each application, what it does and how it may be used in the revenue cycle. There are several companies out there that have developed some good and some not so good AI applications.
We believe having the knowledge of the applications and how they work within the revenue cycle will be helpful when you are making decisions that impact on your department and your healthcare provider.
Some of the examples may sound repetitive in that they are used multiple times; however, you will note that they may use a different AI application. For example, where you may use Speech AI for Patient intake and registration you may also use AI Vision during the registration to translate paper documents to data that can be uploaded to the EHR.
There are multiple examples so it would be beneficial to have the right AI “tools” enhance all your revenue cycle activities.
Speech AI, also known as Speech Artificial Intelligence, refers to technologies that utilize artificial intelligence to enable machines to understand, generate, and interact using human language. It involves two primary fields of study: Natural Language Processing (NLP) and Automatic Speech Recognition (ASR).
Natural Language Processing (NLP): This branch of AI is focused on the interaction between computers and human language. It involves understanding, interpreting, generating, and manipulating human language in a way that is both meaningful and contextually appropriate. This is what allows AI to understand commands, questions, or even write and generate human-like text.
Automatic Speech Recognition (ASR)A: This involves the conversion of spoken language into text. This technology is often used in applications such as voice assistants, transcription services, and any other application where spoken language needs to be understood by a computer.
These technologies, when combined, enable a variety of applications, including but not limited to virtual assistants (like Siri, Alexa, and Google Assistant), speech-to-text transcription services, automated customer service systems, and many more. In all of these, the aim is for the AI to understand and respond to human speech as naturally and accurately as possible.
Patient Intake and Registration: AI can be used to streamline the process of collecting information from new patients or verifying information from existing ones. Speech recognition technology can transcribe spoken data into digital forms, which can reduce administrative workloads and minimize errors. This typically takes the form of an incoming telephone call from the patient interacting with a digital employee who can assist with the registration.
Insurance Verification: Speech AI can interact with patients to gather their insurance information. The AI can understand complex insurance jargon and ask the necessary questions to clarify coverage details, thus ensuring the hospital or clinic has all the necessary information to bill correctly. This most often happens over the phone, an outgoing call, when an eligibility check fails.
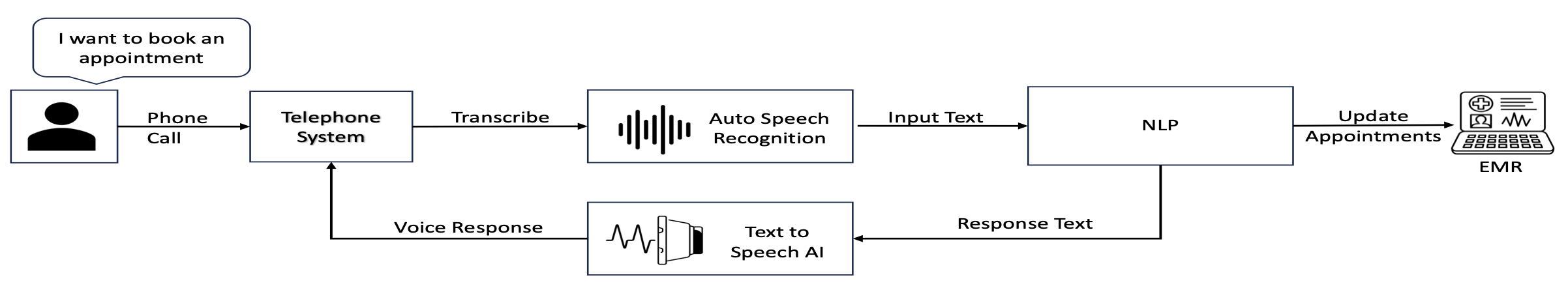
Appointment Scheduling and Reminders: AI can schedule appointments by communicating with patients via phone or text platforms. The AI can also remind patients of upcoming appointments, payment due dates, or necessary actions they need to take before an appointment. This can improve adherence and decrease the number of missed appointments, thus positively impacting the revenue cycle.
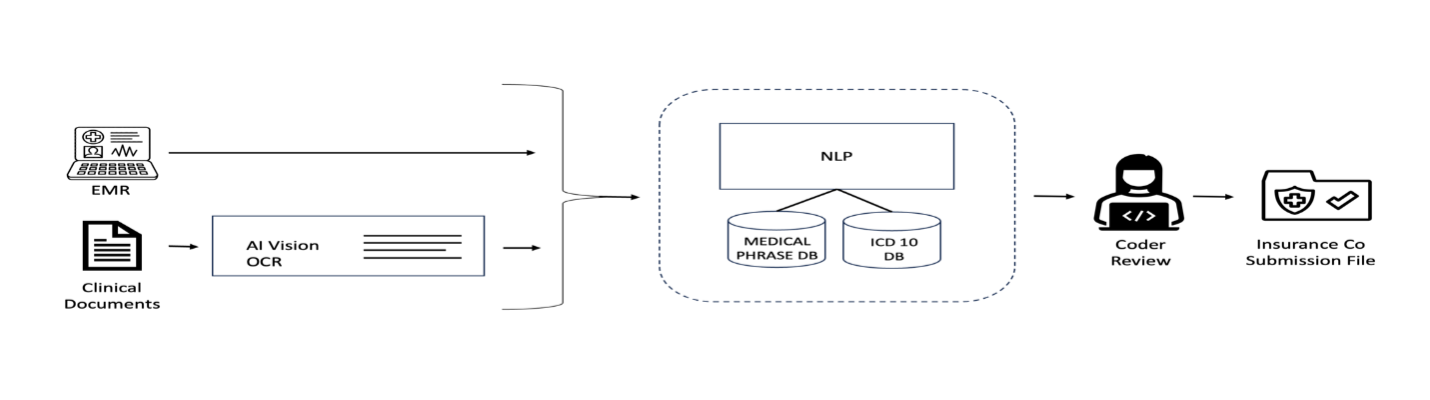
AI VISION (OCR), or Artificial Intelligence Vision Optical Character Recognition, refers to the application of AI technologies, specifically machine learning and computer vision, in the field of Optical Character Recognition (OCR).
Traditional OCR is a technology that is used to convert different types of structured documents, such as scanned paper documents, or PDF files, into editable and searchable data. However, it often struggles with recognizing text in complex layouts or poor-quality images.
AI-enhanced OCR solutions use machine learning algorithms to improve their ability to recognize unstructured text, i.e., having a variety of fonts, colors, layouts, and even on different surfaces. The pattern matching enabled by machine learning allows AI Vision OCR to handle noisy backgrounds, poor lighting conditions, distortions, and other complexities that traditional OCR might struggle with.
Furthermore, by combining AI OCR with Natural Language Processing, these solutions can not only extract text but also understand the context and make sense of the information, just like a human would. This is extremely beneficial in fields like data entry, document analysis, invoice processing, claims submission and many others where manual text extraction could be time-consuming and error prone.
Patient Registration and Data Entry: When patients fill out paper-based forms or submit digital forms with images or PDFs, AI OCR can be used to extract the data and populate it into the Electronic Health Record (EHR) system. This can save time and reduce errors associated with manual data entry.
Insurance Verification: AI OCR can scan and process insurance cards and other related documents. It can extract information like policy numbers, coverage details, and patient identifiers to verify insurance and ensure accurate billing.
Robotic Process Automation (RPA) and Decision Trees work together to enable automated decision-making in business processes.
Decision Trees: A Decision Tree is a type of predictive modeling tool. It uses a tree-like model of decisions and their possible consequences, including chance event outcomes, resource costs, and utility. It is one way to display an algorithm that only contains conditional control statements. In the context of automation, decision trees can be used to map out different outcomes based on a series of decisions, making it a useful tool for scenario analysis.
Robotic Process Automation (RPA): RPA is a technology that uses software robots (or 'bots') to automate repetitive, rules-based tasks usually performed by humans. These tasks can include data entry, transaction processing, and responding to simple customer service queries.
When used together, decision trees provide the decision-making framework that guides the actions of the RPA bots. For instance, an RPA bot might be programmed to take different actions based on the outcomes in a decision tree. Some healthcare Revenue cycle examples of combined decision trees and RPA:
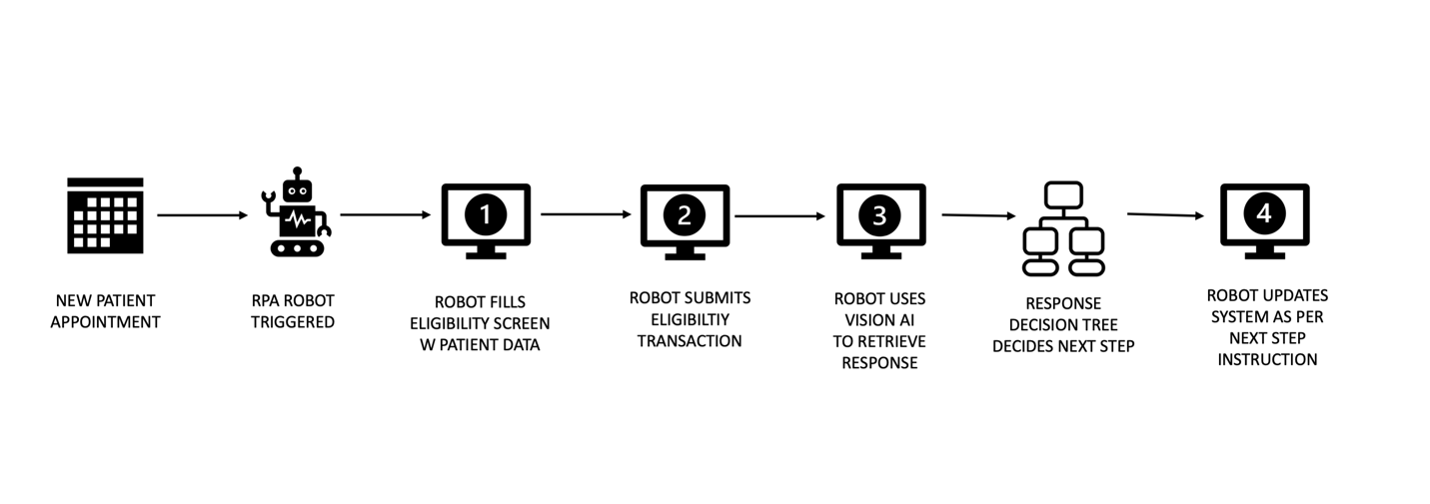
Patient Eligibility Verification: Decision trees can be used to define the sequence of steps to verify a patient's insurance eligibility, while RPA bots can execute these steps. The bot would gather patient insurance details, login into the insurer website and validate them, and then update the patient's profile in the Electronic Health Record (EHR) system.
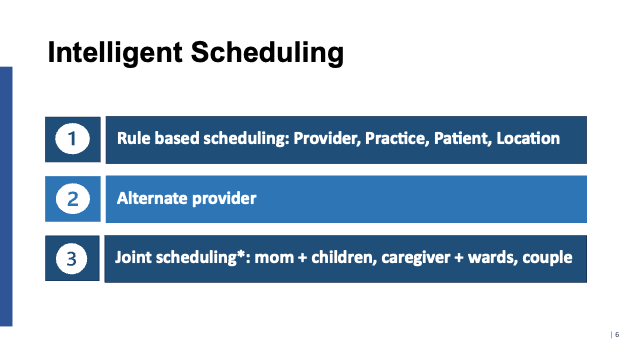
Appointment Scheduling: Decision trees can be used to guide patients through the process of scheduling an appointment based on factors such as their symptoms, the urgency of their condition, and the availability of doctors. RPA bots in conjunction with Speech AI can then automate the actual scheduling process in the EHR system based on the inputs gathered. The interaction with the patient and the review of the EHR scheduling system is done in real time using RPA.
Having a product that can address the historical pain points of lost revenue, lack of staff, underutilization of clinical staff and equipment and the overall inefficiency of operations lends itself to the integration of a “tool kit” to address these issues. A product that can be customized to the unique operations of a healthcare provider and not an “out of the box” solution.
The examples in our Problem Statement provide specific opportunities using AI applications to successfully increase net revenue, repurpose or reduce staff and ensure the utilization of all available clinical staff and equipment.
This all leads to the larger question – Why Digital Employees?
In terms of the integration of applications we focus on what is called UNIFIED A:
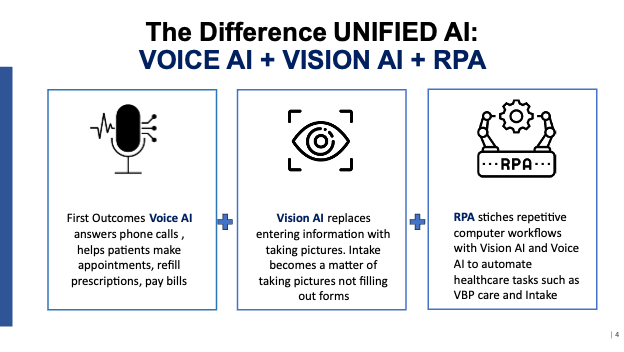

The ability to carry on a conversation with a patient or other individual, while controlling the discussion is extremely important. As pointed out earlier healthcare organizations have specific guidelines to protect the patient information through adherence to HIPPA requirements, Privacy laws and PCI compliance.
The Digital Employee is designed with these guidelines for all application programming. The following are some of the features and functions:
Example 1: A physician only wants to see patients on Tuesdays and Thursdays from 1pm – 4pm as they are in surgery the rest of the time. When a patient calls for an appointment, the digital employee will query the scheduling system specifically for that physician and offer the first available appointment.
If the patient cannot make the first appointment offered, based on your current criteria it will offer other times for the patient until the appointment is made.
Example 2: If a healthcare provider would like to offer screenings for mammograms, prostate, heart, etc. the digital employee can review the EHR to determine the last time the patient had a particular screening and then make an outbound call to the patient to schedule.
With some payers such as Medicare, you can only have a screening every other year or some combination based on their criteria. By reviewing the patient record the digital employee can either call or not based on specific criteria.
As the digital employee can be programmed however the healthcare organization would like to communicate with a patient, department or clinician. While engaged with digital employee programs are running in the background to satisfy the request of the caller.
The current digital employee that is being deployed is as a result of four years of development and continuous improvement. These are not only from a programming perspective, but also from Lean processing to have “waste” free process for the healthcare system before implementation.
The value of patience in adopting emerging technologies is critical to the compliance and success of and implementation of AI applications.
Early adopters of new technologies, most notably those incorporating artificial intelligence (AI) have demonstrated the advantages of a measured and deliberate approach. By thoroughly evaluating each facet of an application and providing constructive feedback, these organizations have helped shape more effective, market-ready products.
Our philosophy draws inspiration from a well-known quote attributed to the U.S. Navy SEALs:
"Slow is smooth, smooth is fast."
This principle encapsulates the value of precision and intentionality:
"Slow is smooth": Deliberate, well-considered action results in greater consistency and fewer errors.
"Smooth is fast": Efficiency stems from well-executed processes, minimizing rework and maximizing productivity.
Applying this mindset to technology adoption—particularly in critical areas like revenue cycle management—helps organizations avoid avoidable failures, reduce operational disruptions, and enhance system performance.
From a revenue cycle standpoint, being an early adopter of proven, vetted solutions can unlock substantial benefits without the volatility that often accompanies untested tools. In short, embracing Seals’ philosophy offers a strategic roadmap to successful implementation and sustainable innovation.
There is no question that AI is here to stay and continues to evolve. Outside of healthcare almost every aspect of business uses some form of AI.
Like the days of paper advertising that “learned” your buying habits, AI applications have taken that practice to a new level suggesting products you may not have thought about or many other “impulse” buying techniques.
The very beginning of this paper focused on revenue generation and cost savings. As healthcare organizations continue to be “squeezed” by reduced payments and more and more regulation and clinical innovation, it is critical that they utilize new technologies to assist them.
Digital employees is a fully developed program that Smart Source, LLC has available and is eager to demonstrate and model the costs, savings and positive applications to your bottom line.